Think about the last time you went to the doctor. You likely saw a nurse, a doctor, and perhaps a specialist or a laboratory technician. Modern healthcare is a team sport.
In fact, over 85% of people in the U.S. see a healthcare professional at least once a year, and many have multiple visits for a single health issue.
For decades, we’ve focused on developing individual doctors and nurses as experts in their respective fields. But we’ve often forgotten to teach them how to be an expert team. This is a significant problem that experts call “coordination neglect”. When healthcare teams don’t work together smoothly, the results can be disastrous: fragmented care, dangerous medical mistakes, and sky-high costs.
This article demonstrates that teamwork is a powerful tool that saves lives, improves patient health, and even reduces costs.

The High Cost of Working in Silos
When healthcare teams don’t communicate or work together, the consequences are serious and measurable. The data demonstrate this in two clear ways: harm to patients and costs to the healthcare system.
The Human Cost: A Patient Safety Crisis
A 2016 Johns Hopkins study found that up to 250,000 people in the U.S. die each year from preventable medical mistakes, making it the third leading cause of death. The shocking truth is that many of these mistakes aren’t caused by a lack of knowledge, but by simple communication breakdowns.
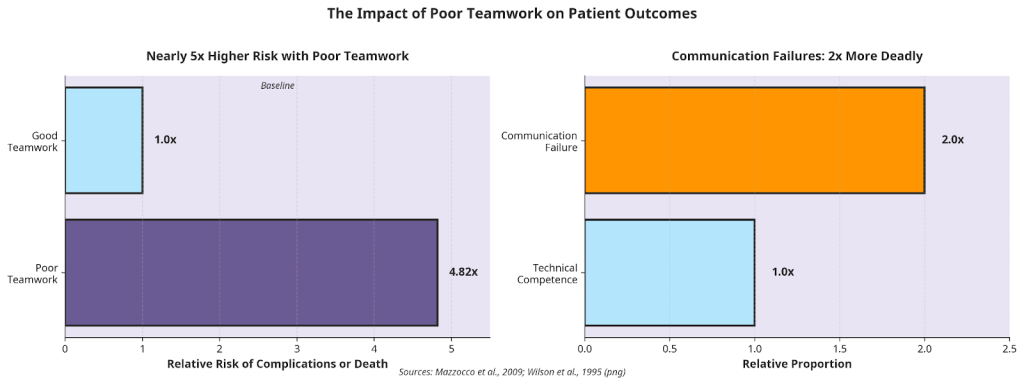
A communication failure is twice as likely to lead to a preventable death as a mistake in a doctor’s technical skill. The numbers are alarming. One study discovered that patients who are treated by a team with poor teamwork are nearly five times more likely to have serious complications or even die.
In fact, simple communication failures are responsible for twice as many preventable deaths as mistakes in a doctor’s or surgeon’s technical skills. These aren’t just abstract numbers. Poor teamwork leads to real-world problems every day in hospitals and clinics.
The Financial Cost: A System Under Strain
Beyond the tragic human cost, poor teamwork is also incredibly expensive. While it costs money to train teams and establish new workflows, the data show that doing nothing costs far more.
One study estimated that the direct cost of providing team-based care is approximately $291 per patient per year. That might sound like a lot, but let’s put it in perspective. For a patient with heart disease, the total cost of care for one year can be over $18,953. The total cost of team-based care is just $356—a tiny 1.9% of the total.
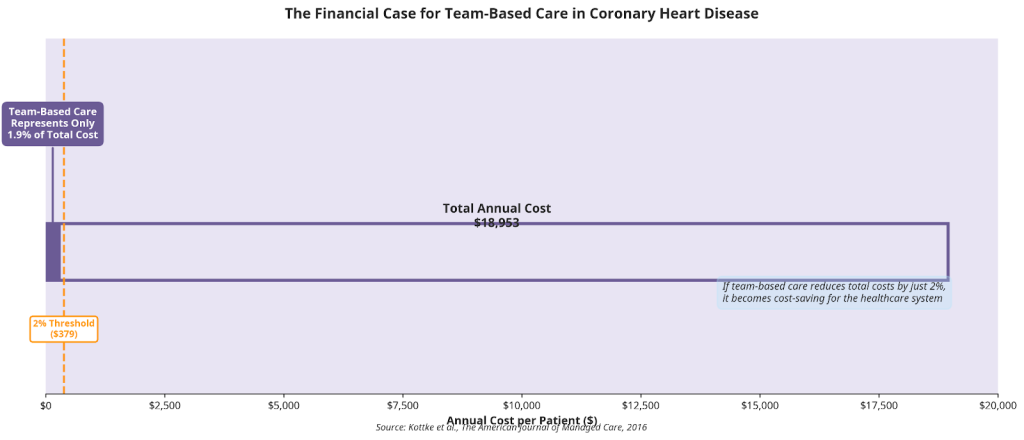
This leads to a powerful conclusion for hospital leaders: a small investment in teamwork
can save a huge amount of money by preventing expensive complications. The same study found that if team-based care reduces the total cost of care by just 2%, it pays for itself and starts saving the system money.
However, the study also found a strange problem with how healthcare is often paid for. Because good teamwork is more efficient (meaning fewer visits and tests), a primary care clinic can actually lose money—about 2.5% of its revenue—by working better. This underscores the importance of adopting a system that rewards quality outcomes, not just the number of procedures.
What Makes a Great Healthcare Team?
So, what does a great healthcare team actually look like? It’s more than just a group of smart people working in the same building. It’s about how they work together.
More Than Just a Group: Two Types of Teams
You might hear the terms “multidisciplinary” and “interdisciplinary” used to describe healthcare teams. They sound similar, but they are very different in practice. An interdisciplinary team is the model that truly puts the patient first.
The 5 Ingredients for a Successful Team
The American Hospital Association has identified five key ingredients for building a successful interdisciplinary team. These are the building blocks for creating a culture of teamwork.
1. Shared Goals: Everyone on the team, from the surgeon to the physical therapist, knows and agrees on what they are trying to achieve for the patient.
2. Clear Roles: Each team member knows exactly what their job is and what they are responsible for. This avoids confusion and ensures no tasks fall through the cracks.
3. Mutual Trust: Team members feel safe to speak up, ask questions, and even admit mistakes without fear of being blamed. This “psychological safety” is essential for catching errors before they harm a patient.
4. Effective Communication: The team has simple, reliable ways to share information quickly and clearly. Everyone has the information they need when they need it. Modern teams are increasingly moving toward dedicated clinical collaboration platforms like HosTalky to ensure that critical patient data isn’t trapped in a silo but is available to every team member in real-time.
5. Shared Processes and Results: The team regularly looks at how well they are working together and whether they are achieving their goals. This enables them to continually learn and improve.
Read more on effective communication in How to Master Therapeutic Communication in Nursing
Real-World Stories of Transformation
These ideas about teamwork aren’t just theory. Across the country, top hospitals are applying these principles to deliver significant improvements in patient care.
Case Study 1: Virginia Mason – A Revolution in Patient Care
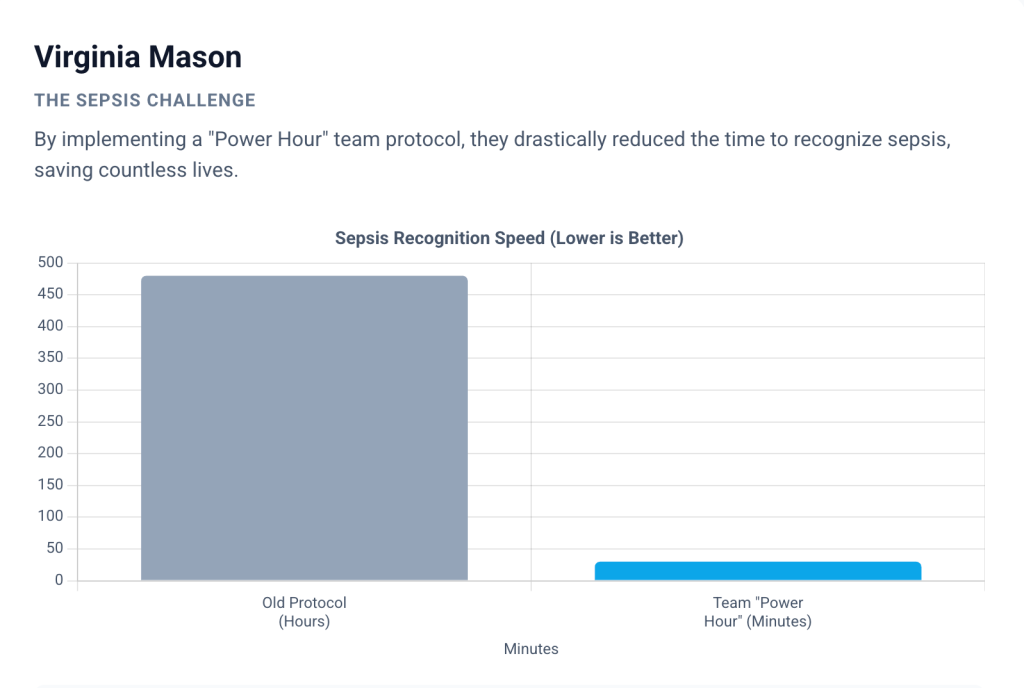
Back in 2002, the Virginia Mason healthcare system in Seattle decided to make a radical change. They borrowed ideas from Toyota, the ultra-efficient car company, to create the “Virginia Mason Production System.” Their goal was to provide the “perfect patient experience” by empowering their staff to fix problems themselves.
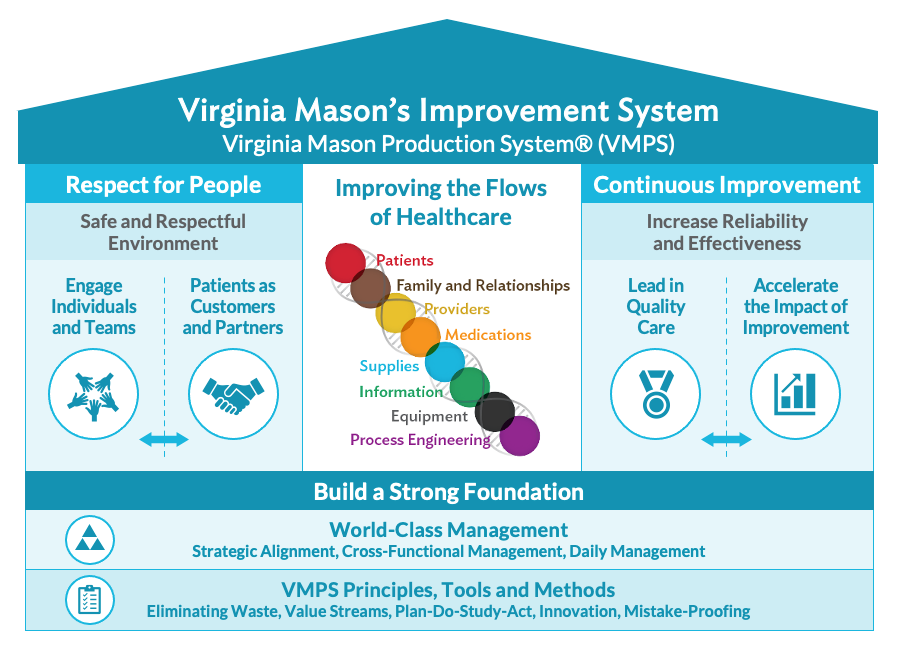
“The team members who do the work know what the problems are, and have the best solutions.”‒ The Virginia Mason Philosophy
The results have been nothing short of amazing:
- Fighting Sepsis: Sepsis is a life-threatening reaction to infection. By implementing a team-based “Power Hour” protocol, Virginia Mason reduced the time to sepsis recognition from 8 hours to 30 minutes. This is saving lives
- A Safer Hospital: They created a “Patient Safety Alert” system that allows any employee to stop a process if they see something that could harm a patient. More than 120,000 safety alerts have been filed, making the hospital much safer and reducing lawsuits by.
- Tackling the Opioid Crisis: Using their teamwork method, they were able to achieve a 30% improvement in reducing large, high-dose initial opioid prescriptions, helping to fight the opioid epidemic in their community.
Case Study 2: Johns Hopkins – A Safety Model for the Nation
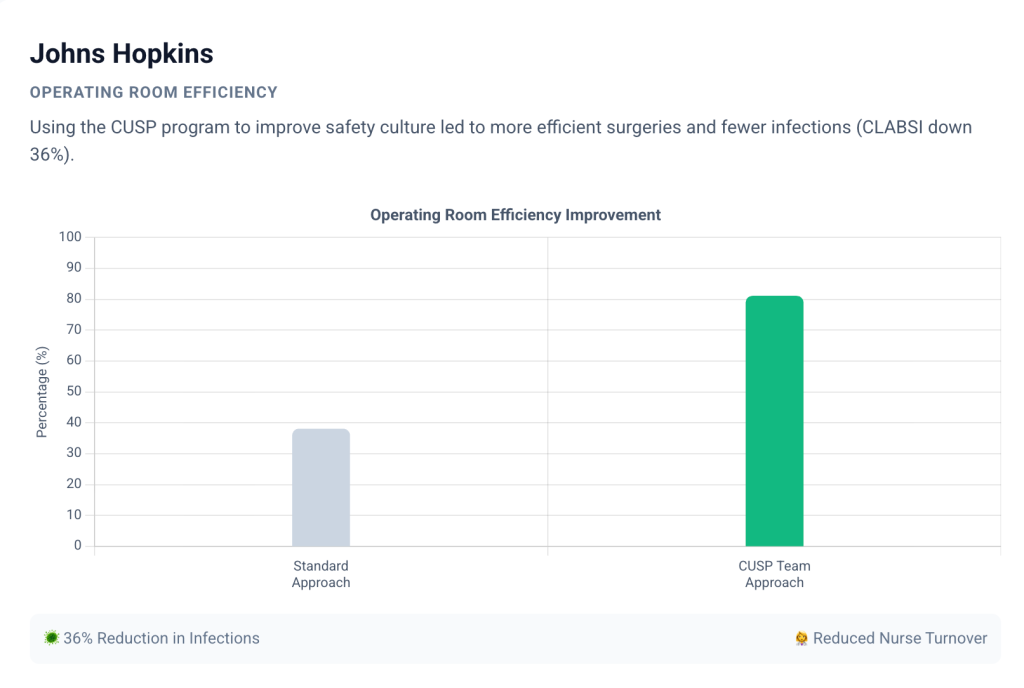
Researchers at the world-famous Johns Hopkins Hospital created the Comprehensive Unit-based Safety Program (CUSP). It’s a step-by-step guide that helps frontline staff improve safety culture and solve problems in their own units.
The program has been so successful that it’s now used in hospitals in all 50 states. CUSP works by teaching teams to identify risks, learn from errors, and work more effectively together. The results speak for themselves:
- More Efficient Surgery: At one hospital, using CUSP for complex spine surgery more than doubled the number of surgeries that started on time, from 38% to 81%. This means less waiting for patients and a more efficient operating room.
- Fewer Infections: In a large-scale project across more than 1,000 Intensive Care Units (ICUs), the CUSP program achieved a 36% reduction in central line-associated bloodstream infections (CLABSI).
- Happier Staff: One study found that after implementing CUSP, nurses reported a better safety and teamwork climate in their unit. It even reduced nurse turnover, meaning experienced staff were more likely to stay.
Teamwork in Action Everywhere
The benefits of teamwork aren’t limited to big hospitals. The American Speech-Language Hearing Association (ASHA) shares stories of how teamwork makes a difference in all kinds of settings :
- Stroke Recovery: A team of therapists worked together to help a young woman who had a stroke learn to live independently again.
- Helping Children: A team of specialists, including surgeons and therapists, collaborated to help a baby with a cleft palate learn to eat and speak properly.
- Training Future Heroes: A university created a realistic tornado simulation to teach students from nursing, medicine, and other health programs how to work together during a crisis.
The Bottom Line: Teamwork Pays Off
For any hospital or clinic, money matters. The good news is that investing in teamwork isn’t just good for patients; it’s good for the bottom line, especially as healthcare moves toward paying for quality over quantity.
As we saw, the cost of team-based care is small compared to the enormous cost of
complications from poor care. When teams work well together, they prevent expensive problems like:
- Costly emergency room visits
- Unnecessary hospital readmissions
- Long, expensive hospital stays
- Wasteful or repeated tests
This is where we see the 2% Tipping Point. Remember, if investing in teamwork can reduce the total cost of care by just 2%, it pays for itself and starts saving the entire system money. Implementing a centralized hub provides the operational visibility needed to streamline patient flow and reduce the length of stay, directly contributing to that 2% savings threshold.
In a world of rising healthcare costs, an investment that can improve care and Reduce Costs is a clear winner.
“Until savings are shared, the additional cost of team-based care will be a barrier to the adoption of the strategy by primary care practices.”‒ Kottke, T. E., et al., The American Journal of Managed Care
This quote highlights the challenge: we need to ensure that hospitals and clinics that excel at working as a team are rewarded for it. That’s the future of healthcare finance.
A Roadmap for Building a Culture of Teamwork
So, how can your organization start building a culture of teamwork? It’s a journey, but you can start today. Here are five steps based on the lessons from the world’s most successful healthcare teams.

Step 1: Get Leaders on Board
Change has to start at the top. Hospital leaders need to prioritize teamwork. They need to provide the resources, remove roadblocks, and lead by example.
Step 2: Start Small and Get a Win
Don’t try to change the whole hospital at once. Pick one unit or one project to start with. When you show that teamwork can make a real difference on a small scale, it will be much easier to get everyone else on board.
Step 3: Empower Your Frontline Staff
The best ideas for improvement often come from the people doing the work every day. Give your nurses, therapists, and technicians the training and authority to spot problems andtest solutions. Trust them to improve their work.
Step 4: Measure Your Progress
You can’t improve what you don’t measure. Track your progress with a simple dashboard that everyone can see. Measure things like infection rates, patient falls, and patient satisfaction scores to see the impact of your teamwork initiatives.
Step 5: Invest in Training
Teamwork is a skill, and like any skill, it can be learned. Invest in training programs that teach your staff how to communicate clearly, resolve conflicts, and make decisions as a Team.
Check out: 5 Fun Team-Building Exercises for Healthcare Professionals
Conclusion: The Future of Healthcare is a Team Sport
The evidence is clear. In our complex modern world, the single best way to make healthcare safer, more effective, and more affordable is to focus on teamwork. The data shows that working in silos leads to preventable tragedies and wasted money. In contrast, working together saves lives, improves the patient experience, and makes financial sense.
The stories from hospitals like Virginia Mason and Johns Hopkins are not miracles; they are blueprints for a better way. They show that when you commit to a culture of collaboration and empower your teams, you can achieve amazing results.
As we move toward a future of healthcare that values quality over quantity, one thing is certain: the best hospitals will be the ones that understand that healthcare is, and always will be, a team sport.
The Next Step for Your Team.
Transitioning from “coordination neglect” to an expert team requires both a cultural shift and the right toolkit. If you’re ready to dismantle the silos in your organization, HosTalky provides the HIPAA-compliant framework for the interdisciplinary collaboration described in this article.
Stop communication breakdowns before they impact patient safety. Explore HosTalky’s secure, healthcare-first coordination tools here.
References:
- Rosen, M. A., DiazGranados, D., Dietz, A. S., Benishek, L. E., D’Innocenzo, L., Landon, B., & Pronovost, P. J. (2018). Teamwork in healthcare: Key discoveries enabling safer, high-quality care. American Psychologist, 73(4), 433‒450.
- Heath, C., & Staudenmayer, N. (2000 ). Coordination neglect: How lay theories of organizing complicate coordination in organizations. Research in Organizational Behavior, 22, 153‒191. https://doi.org/10.1016/S0191-3085(00 )22005-4
- Makary, M. A., & Daniel, M. (2016). Medical error—the third leading cause of death in the US. The BMJ, 353, i2139.
- Mazzocco, K., Petitti, D. B., Fong, K. T., Bonacum, D., Brookey, J., Graham, S., … & Thomas, E. J. (2009 ). Surgical team behaviors and patient outcomes. The American Journal of Surgery, 197(5), 678-685.
- Wilson, R. M., Runciman, W. B., Gibberd, R. W., Harrison, B. T., Newby, L., & Hamilton, J. D. (1995 ). The Quality in Australian Health Care Study. Medical Journal of Australia, 163(9),458-471.
- Gawande, A. A., Zinner, M. J., Studdert, D. M., & Brennan, T. A. (2003). Analysis of errors reported by surgeons at three teaching hospitals. Surgery, 133(6), 614-621.
- Klevens, R. M., Edwards, J. R., Richards, C. L., Jr., Horan, T. C., Gaynes, R. P., Pollock, D. A., & Cardo, D. M. (2007 ). Estimating health care‒associated infections and deaths in U.S. hospitals, 2002. Public Health Reports, 122(2), 160‒166.
- Miake-Lye, I. M., Hempel, S., Ganz, D. A., & Shekelle, P. G. (2013). Inpatient fall prevention programs as a patient safety strategy: A systematic review. Annals of Internal Medicine, 158(5Part2), 390-396.
- Newman-Toker, D. E., & Pronovost, P. J. (2009 ). Diagnostic errors—the next frontier for patient safety. JAMA, 301(10), 1060‒1062.
- Lyu, H., Wick, E. C., Housman, M., Freischlag, J. A., & Makary, M. A. (2013 ). Patient satisfaction as a possible indicator of quality surgical care. JAMA Surgery, 148(4), 362‒367.
- Kottke, T. E., Maciosek, M. V., & Huebsch, J. A. (2016 ). The financial impact of team based care on primary care. The American Journal of Managed Care, 22(8), e283-e286.
- American Hospital Association. (2020). Team-Based Care Creates Value. AHA Value Initiative Issue Brief.
- Virginia Mason Franciscan Health. (n.d. ). VMPS Success Stories. Retrieved January 31, 2026, from Johns Hopkins Medicine. (n.d. ). CUSP Implementation Training. Armstrong Institute for Patient Safety and Quality. Retrieved January 31, 2026, from Raman, D. L., Bixby, E. C., Wang, K., Rossi, D., Ringler, J., Wiggins, D. A., … & Vitale, M. G. (2022 ). A Comprehensive Unit-based Safety Program to Improve Perioperative Efficiency in Adolescent Idiopathic Scoliosis. Journal of Pediatric Orthopaedics, 42(3), 123-130.
- Latif, A., et al. (2024). Implementation and long-term efficacy of a multifaceted intervention to decrease central line-associated bloodstream infections in adult intensive care units in Saudi Arabia. American Journal of Infection Control.
- Timmel, J., Kent, P. S., Holzmueller, C. G., Paine, L., Schulick, R. D., & Pronovost, P. J. (2010 ). Impact of the Comprehensive Unit-based Safety Program (CUSP) on safety culture in a surgical inpatient unit. The Joint Commission Journal on Quality and Patient Safety 36(6), 252-260. https://doi.org/10.1016/S1553-7250(10 )36040-5
- American Speech-Language-Hearing Association. (n.d.). Interprofessional Education/Interprofessional Practice (IPE/IPP) Case Studies. Retrieved January 31, 2026