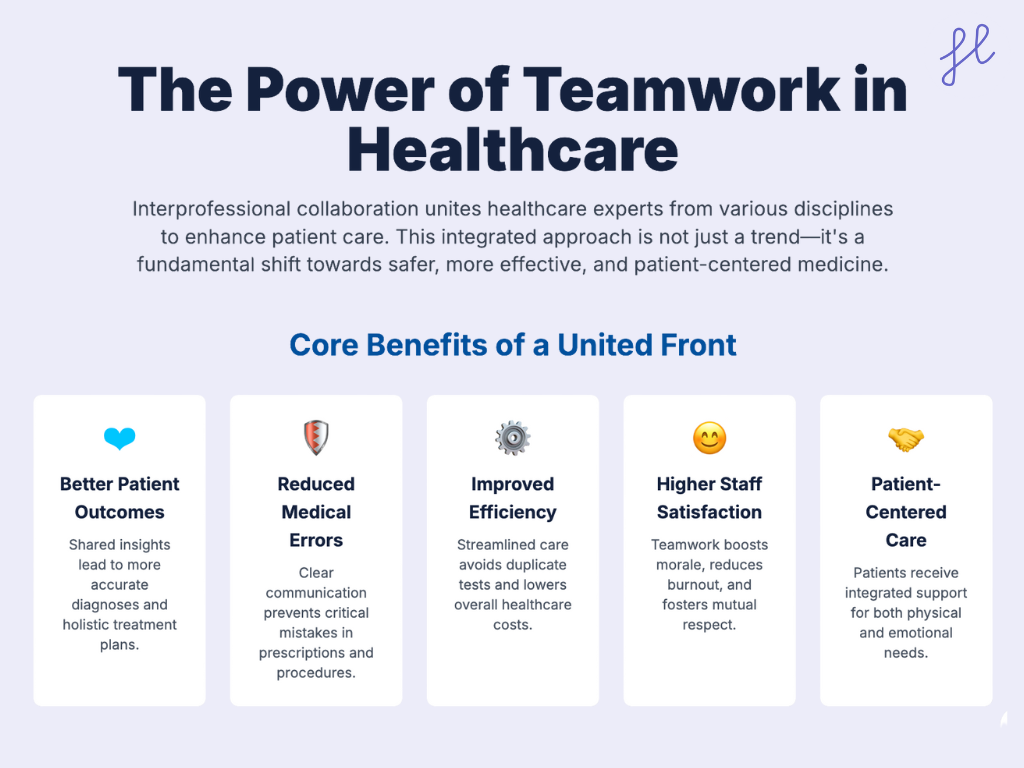
Healthcare is no longer the work of a single professional. Patients today present with complex needs—chronic illnesses, mental health concerns, and lifestyle factors that require more than one perspective. This is where interprofessional collaboration in healthcare comes in.
Bringing together doctors, nurses, pharmacists, therapists, social workers, and other professionals, interprofessional collaboration (IPC) reduces errors, improves outcomes, and helps healthcare systems run more efficiently.
In this blog post, we’ll explore 10 of the best examples of interprofessional collaboration in healthcare so you can better understand how you can implement this in your team too!
What Is Interprofessional Collaboration in Healthcare?
Interprofessional Collaboration in Healthcare refers to different healthcare professionals (such as doctors, nurses, pharmacists, etc.) working together to provide coordinated, high-quality patient care. The benefits of interprofessional collaboration in healthcare are immense.
It involves effective verbal cues in communication, mutual understanding of each profession’s roles, and a shared commitment to patient well-being.
Unlike multidisciplinary care—where providers work separately but in parallel—interprofessional collaboration emphasizes communication, shared decision-making, and joint accountability for patient outcomes.
Recent innovations such as telehealth platforms, electronic health records (EHRs), and AI-driven decision support systems have further expanded opportunities for collaboration across locations and specialties.
How does this work? Well, we have case-to-case practical examples of interprofessional collaboration below, so check them out.
What is Another Word for Interprofessional Collaboration?
Another word for interprofessional collaboration is team-based care. Other alternatives include:
- Multidisciplinary collaboration (though slightly different, it emphasizes multiple disciplines working together)
- Collaborative care
- Integrated healthcare teamwork
- Interdisciplinary teamwork
10 Interprofessional Collaboration in Healthcare Examples
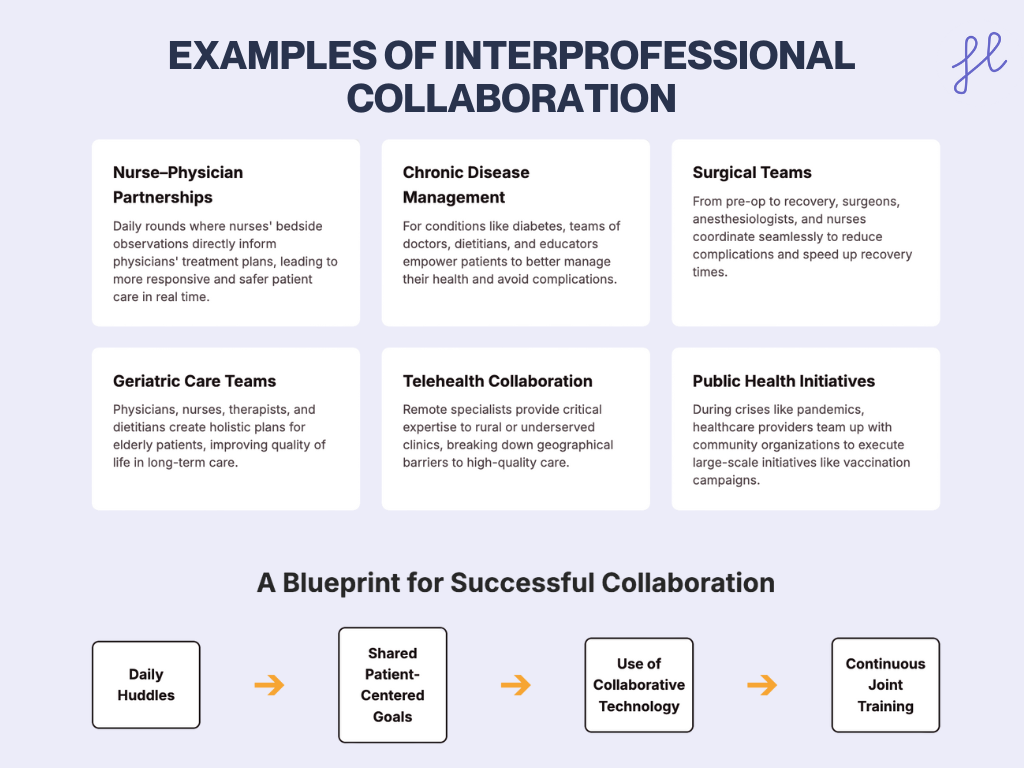
Nurse–Physician Partnerships
Nurses often spend the most time at the patient’s bedside, while physicians oversee diagnosis and treatment planning. When they collaborate effectively, patient care becomes more responsive and safer.
- How it works: Nurses identify subtle changes in a patient’s condition and communicate them directly to physicians. Doctors then adjust care plans in real time.
- Example: In ICU settings, nurse-physician daily “rounds” ensure that both clinical expertise and frontline observations shape treatment.
A 2024 study in SAGE Open Nursing found that enhanced nurse-physician collaboration led to improved patient outcomes and reduced medical errors in hospital settings. SAGE Journals
Read more on: Why Teamwork Matters in Healthcare: Data, Stories & Solutions
Managing Chronic Conditions
Imagine a patient diagnosed with diabetes. A team comprised of a doctor, nurses, a registered dietitian, and a social worker springs into action. The doctor prescribes the necessary medication, while the nurses provide education on injection techniques and blood sugar monitoring.
The dietitian tailors a meal plan to manage blood sugar levels, and the social worker assesses for any social or emotional challenges that might affect the patient’s ability to manage their diabetes.
Not only that, there are popular healthcare apps used by busy healthcare professionals to help them work collaboratively with their colleagues.
Stroke Care Team
At a leading stroke center, an interprofessional team comprising neurologists, emergency medicine physicians, nurses, physical therapists, occupational therapists, and speech-language pathologists can collaborate to provide exceptional stroke care.
The team meets regularly to discuss patient cases, share their expertise, and coordinate the delivery of evidence-based treatments and rehabilitation services.
Impact: This collaborative approach can lead to improved patient outcomes, reduced hospital stays, and a higher rate of functional independence for stroke survivors.
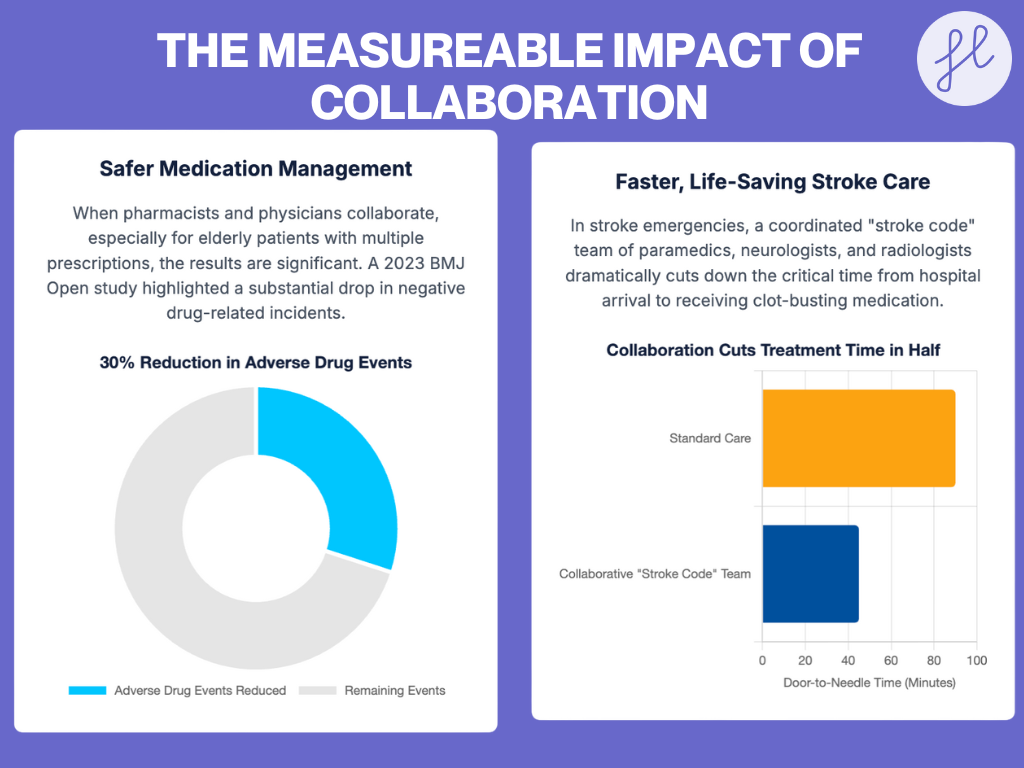
Pharmacist–Physician Collaboration
Pharmacists work directly with physicians to manage medications, minimize side effects, and prevent adverse drug interactions, especially in polypharmacy cases for elderly patients.
Example: In polypharmacy cases for elderly patients, pharmacists collaborate with doctors to “deprescribe” unnecessary medications and adjust dosages.
A 2023 BMJ Open study found that pharmacist-physician teams lowered adverse drug events by nearly 30% in outpatient clinics.
Post-Surgical Care
Following surgery, a patient’s journey to recovery is significantly smoother with a collaborative team by their side. The surgeon ensures the success of the operation, while the nurses provide pain management and monitor vital signs.
A physical therapist guides the patient through exercises to regain mobility and strength, while an occupational therapist helps them relearn daily tasks.
Impact: This collaboration ensures all aspects of recovery are addressed and avoids all common healthcare communication errors in the workplace.
Check this out: Best Strategies to Prevent Common Medical Errors
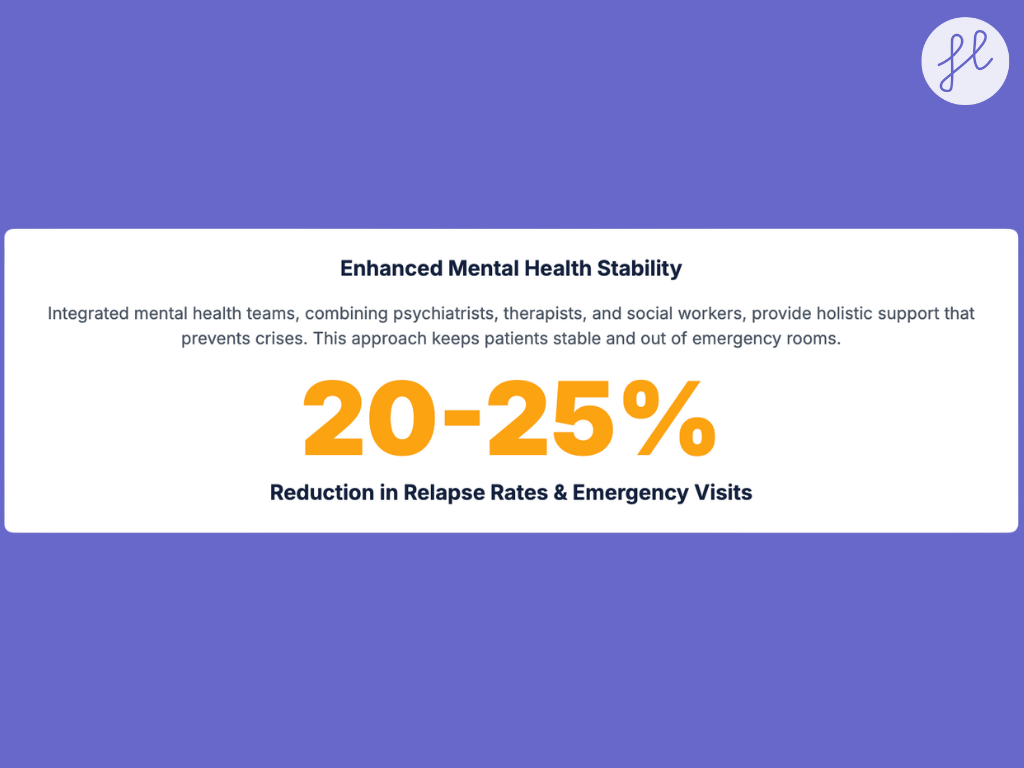
Mental Health Care
Depression is a complex condition, and a collaborative approach is key to effective treatment. A team of psychiatrists who can prescribe medication, psychologists or therapists who provide therapy sessions, and social workers who address social support systems work together to create a holistic treatment plan.
Example: Community-based mental health teams often coordinate to support patients with severe depression—combining medication, counseling, and social support (housing, employment).
Telehealth Collaboration
Geographic limitations shouldn’t hinder access to specialized care. Telehealth technology bridges this gap by allowing doctors in remote areas to consult with specialists in urban centers.
Example: A rural clinic treating a child with a rare cardiac condition connects with a pediatric cardiologist hundreds of miles away, who advises in real time.
You can also check out this blog, which compares Telehealth vs Telemedicine.
Read more on: Telehealth vs Telemedicine vs Telecare
Pain Management Team
Chronic pain can be debilitating, and managing it effectively requires a collaborative effort. Doctors, nurses, and pharmacists work together to develop a safe and effective pain management plan for the patient. The doctor considers the underlying cause and prescribes appropriate medication.
Nurses provide education on chronic and acute pain management techniques and monitor side effects. Pharmacists review medications for interactions and ensure patients understand how to take them safely.
Additionally, the team might explore alternative therapies like physical therapy or acupuncture, offering a more comprehensive approach to pain relief.
Palliative Care Team
For terminally ill patients and their families, a palliative care team provides invaluable comfort and support. Doctors manage pain symptoms, nurses offer emotional and physical care, social workers address social and practical concerns, and spiritual care providers offer guidance and support.
Impact: This collaborative approach ensures the patient’s well-being is addressed from all angles, allowing them to face the end of life with dignity and peace.
Also read SBAR And Other Effective Communication Tools In Nursing
Geriatric Care Teams
Elderly patients benefit from collaboration between physicians, nurses, dietitians, physical therapists, and caregivers, ensuring holistic support.
Example: In long-term care facilities, “care conferences” bring together doctors, nurses, therapists, and family members to align on treatment plans.
A 2023 study in BMC Geriatrics described the development of geriatric rehabilitation care teams towards interprofessional collaboration, leading to improved patient outcomes. BioMed Central
Medication Management
Especially for patients with multiple prescriptions, medication management becomes crucial. Pharmacists collaborate with nurses and doctors to review medications for potential interactions and ensure they are taken correctly.
They can also identify potential medication adherence issues and educate patients on proper medication use.
Impact: This collaboration helps to avoid adverse reactions and ensures patients receive the full benefits of their medications.
Wound Care Team
Chronic wounds can be a significant challenge. A wound care team comprised of doctors, nurses, and specialized wound care experts works together to develop a comprehensive treatment plan.
They consider factors like appropriate dressings, effective wound therapies, and even nutritional support to promote healing.
Impact: This collaborative approach increases the chances of successful wound closure and improved patient outcomes.
Maternal and Child Health
Bringing new life into the world is a journey that benefits from a collaborative team. Obstetricians provide prenatal care and manage the delivery process. Pediatricians take over after birth, ensuring the newborn’s health and development. Nurses provide constant care and support for both mother and baby. Lactation consultants offer guidance on breastfeeding, promoting a healthy start for the newborn.
Impact: This collaboration ensures a smooth and supportive journey for mothers and their newborns.
Emergency Response Teams
In emergency departments, doctors, nurses, paramedics, and specialists make split-second decisions as a unit—saving lives during trauma and critical cases.
Example: In stroke care, ER teams follow a “stroke code,” where paramedics alert hospitals in advance, neurologists are on standby, and radiologists expedite CT scans.
Impact: Streamlined collaboration can reduce door-to-needle time for clot-busting medication from 90 minutes to under 45 minutes—significantly improving survival and recovery outcomes.
A 2024 systematic review in Trauma Surgery & Acute Care Open found that trauma care and emergency preparedness training programs significantly enhance prehospital primary survey effectiveness and team performance. PMC
Community Outreach Programs
Healthcare doesn’t happen solely within hospital walls. Healthcare professionals often collaborate with community organizations to address social determinants of health the social and economic factors that influence health outcomes.
For instance, they might partner with schools to provide immunization clinics and other clinic services to offer mental health services in underserved areas.
Impact: This collaborative approach extends healthcare’s reach and promotes a healthier community overall.
Public Health Initiatives
During COVID-19 vaccine rollouts, healthcare providers worked with schools, local governments, and NGOs to set up mass vaccination sites and outreach campaigns.
Evidence: A 2023 study in the Journal of Public Health Management and Practice highlighted the effectiveness of community-based collaborations in addressing mental health during the COVID-19 pandemic, improving holistic health outcomes. pcori.org
Impact: Collaborative public health initiatives have led to increased vaccine uptake and better management of health crises.
Best Practices to Foster Effective Collaboration
- Daily Huddles & Team Meetings – Short check-ins align team members and clarify responsibilities.
- Shared Goals & Accountability – Everyone must agree on patient-centered objectives.
- Collaborative Technology – Secure messaging, shared dashboards, and AI-powered tools improve coordination.
- Continuous Training – Simulation exercises, workshops, and joint educational programs build trust and teamwork.
Continue your journey, learn more about Interprofessional Collaboration in Healthcare here:
- What AI Can (And Can’t) Do for Healthcare Communication
- 5 Best Remote Collaboration Tools for Nursing Units
- How to Break Medical Hierarchies to Foster Team Collaboration
FAQs on Interprofessional Collaboration
Interprofessional collaboration enhances health and wellness by bringing together different healthcare professionals to coordinate care, thereby preventing errors, accelerating recovery, and improving patient outcomes.
To provide safe, effective, and patient-centered care through teamwork across healthcare disciplines.
By improving communication, reducing errors, and ensuring multiple professionals review and contribute to care plans.
Communication breakdowns, professional hierarchies, and lack of standardized training.
Multidisciplinary care involves parallel contributions from different professionals, while interprofessional care emphasizes shared decision-making and true collaboration.
Conclusion
Interprofessional collaboration is crucial for delivering the highest quality care to patients within the healthcare system. While implementing true interprofessional collaboration comes with its communication challenges, the benefits to patient outcomes, provider satisfaction, and overall system efficiency make it a crucial priority.
As medical knowledge and treatment options continue to become more complex, interprofessional collaboration will become even more vital for ensuring high-quality, cost-effective care.
Stay informed on the latest healthcare trends, news, and AI advancements. Join us on LinkedIn and Instagram for more updates!